INTRODUCTION
Back pain and neck pain are extremely common. It is the driving force behind disability, at a cost to our society totaling billions of dollars in treatment and lost productivity costs every year.
Lower back pain, specifically, is the number one cause of years lived with disability—in the world. Neck pain ranks in at number four.
When these types of pain present themselves, often interfering with our daily lives, naturally we search for answers. However, an abundance of information can cause confusion over what’s wrong with us, as well as which treatments might help. We start to think we need x-rays, or CT and MRI scans of our spine to “see what’s wrong.”
While scans are appropriate for detecting serious causes of pain, these kinds of cases actually make up less than 1% of all spinal pain!
The Problem With Seeking X-Rays and Scans
Below is a list of the typical findings seen on x-rays and scans in the spines of anyone over 25 years old:
- Disc degeneration arthritis
- Bone spurs
- Stenosis (narrowing)
- Disc bulges and protrusions
These findings occur both in people with and without back pain! In fact, oftentimes a person’s x-ray or scan does not match their symptoms. Many people have advanced signs of disc deterioration and arthritis in their spine yet experience minimal or no pain. Pain changes from day-to-day, but x-ray and scans results do not. Most of the findings on your x-ray and scans have taken years to develop, and offer a look at your health history; but, they may have little bearing on your pain today.
This is because scans show your anatomy, not your pain. And our anatomy naturally changes over time—we expect it to. You can see it on the outside by looking in a mirror, but it’s happening on the inside too. It’s a normal part of life. Does your face hurt from the wrinkles that have developed over the years? Probably not, and that's because ageing is not always painful.
A recent study found that having a CT or MRI scan of your spine may actually increase the chance of having a worse outcome! This was the result of forgoing valuable treatment and rehab time in lieu of waiting for specialist appointments (which are often underwhelming and disappointing to most patients). Despite the allure of a “permanent fix,” surgery is rarely the answer.
Suffice to say: you can’t take a picture of pain. At least not yet. And that is because pain is a very complex process involving your spine, nervous system, and brain.
The Most Overlooked Issue
You have a weak link. And we have a good idea where that is.
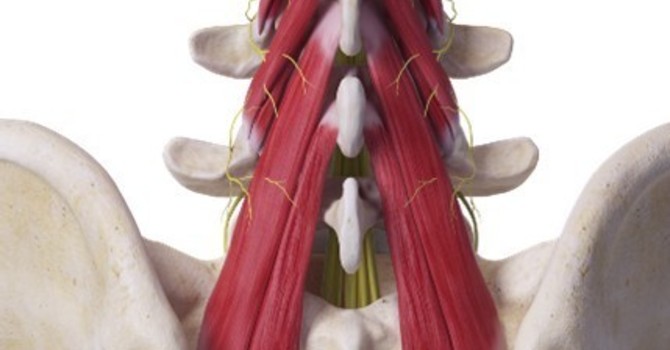
Your small spinal-stabilizing muscles are weak and underperforming.
The multifidus muscle is a major stabilizer located between each vertebra. Studies repeatedly show profound changes in this muscle in up to 95% of MRI scans for chronic whiplash, and neck and back pain. These MRI scans also typically show ‘fatty infiltration of the multifidus’ (and other stabilizing muscles), which is a sign of muscle degeneration. While this is not usually mentioned in your scan report; it’s probably the most important finding—and the one thing that you can do something about. (It also bears repeating: if this finding is present in up to 95% of people with chronic whiplash, neck pain and back pain, you really don’t need a scan to diagnose it…)
Load-Capacity-Pain
There’s a concept we discuss at Edgemont Chiropractic Clinic called “Load-Capacity-Pain.” The principle is simple: if your load (activity) exceeds your capacity (strength), then pain may result. It may manifest from an actual injury, or it may just be your vigilant nervous system giving you a warning sign that you’re about to reach your strength capacity.
It helps to think of pain as an alarm bell. However, pain does not always mean there’s been tissue injury or damage. What's more, your nervous system can become sensitized from previous episodes of back and neck pain, making it more liable to sound the alarm before an injury does occur.
For many people, just sitting all day puts more load on their back that it can tolerate; this inactivity creates pain and muscle tightness. You can think of it as your brain yelling at you to get up and get moving.
Really, pain can result from a number of causes. For some, it’s doing a 1-2-hour walk on the weekend. For others, it’s standing in the kitchen or walking slowly that overloads their muscle capacity. This may surprise you, but standing and slow walking both place more compressive load on the spine than brisk walking does.
You could change your load (do less), or…better still…increase your capacity!
Increase Your Capacity
A fundamental principle of the human body is that physical stress causes adaptation. So let’s get started.
First, think of an activity that you like to do. It could be walking, gardening, tennis, golf, or some other activity. Then, plan to do it for 30 minutes at least three times per week.
Any exercise or activity will usually do. That being said, we always recommend informing us about your chosen exercise program so that we can be sure that you haven’t chosen an activity that may place undo stress on your spine. (You may also benefit from our recommendation of some exercises specific to your problem.)
To further increase your capacity, at least one hour of strength training twice a week is needed. Don’t think of this plan as a day of dedicated back, chest, or arm and leg exercises. Instead, understand that it’s your whole body that needs integrated functional strength training.
Rest days are imperative, too. Muscles get stronger the day after your activity. Give them some time.
Functional Strength Training
We also call this ‘farm boy/farm girl’ strength; or, whole body strength. Your exercise program should include these functional and fundamental movement patterns:
- Squatting
- Lunging
- Hip hinging
- Pushing
- Pulling
- Loaded carries
- Diaphragmatic breathing
- A few specific back/neck exercises as required
You don’t need to lift a ton to do them! That’s because these are the movements you use in your daily life. You don’t use a bench press or leg press motion too often in daily life. The same is true for sit-ups and crunches; they are not functional movements and are potentially harmful to your back.
If you are getting older, you are losing muscle at an increasing rate with every passing year. You can’t stop the hands of time, but you can stop yourself from becoming frail. You must do some strength training to accomplish this. In fact, research shows that 20-30 years of muscle wasting can be reversed in 2-3 months of supervised weight training.
Overdoing core exercises and stretches may also be part of your problem. We give you permission to limit the time that you’re spending training your core. (Yes, it’s important—but it’s also overrated). Instead, simply learn how to breathe properly to activate your core. It’s true—your diaphragm is one of the body’s most important and underutilized core muscles. Learning how to turn on your core and then how to turn it off is key, and a strategy well-known to top athletes. (The same goes for many stretches – not only are they over-emphasized, but they can also actually increase your pain later in the day!)
What you do need for functional strength training is optimized mobility in some of your joints–this means complete and effortless movement. You also need stability—strong muscular control—around other joints.
These Joints need to be strong and stable:
- Feet
- Knees
- Lower back
- Neck
These joints need to be flexible and mobile:
- Ankles
- Hips
- Mid back
- Shoulders
An additional benefit to strength training is its superiority over aerobic exercise in providing some protection from ageing-associated cognitive decline.
Another essential component of functional strength training is getting good sleep. Sleep helps the body in many ways: it facilitates healing and decreases our sensitivity to pain by lowering inflammation levels— this aids the repair process in muscles and in the brain. Sleep also helps to lessen the emotional stress that can amplify pain signals. to lessen the emotional stress that can amplify pain signals.
Should You Exercise When You Have Pain?
Pain is a complex process—it simply cannot be relied upon to help us decide if we’ve actually incurred an injury. And what’s true is that sometimes when we exercise, we hurt. Here’s our Exercise Stoplight Guide to help you decide whether it’s safe to carry on with your activity, or if you should slow it down or stop.
- Stop if your pain increases and there is a 50% or more loss of flexibility after your activity.
- Proceed with caution if your pain increases and persists after your activity, but there is no loss of flexibility. Reduce the frequency, duration or repetitions of your activity instead of ceasing it altogether.
- Keep going if your pain increases but there is no loss of flexibility after the activity, and the pain decreases to baseline shortly after the activity.
CONCLUSION
In general, it's considered safe to move and exercise with back and neck pain present. Any type of activity seems to help, but there are certain principles of movement that should be followed.
Specific exercises unique to your problem often need to be added to an exercise program—and some exercises may need to be removed. Your stress, mood, and sleep habits ,all play a big role in “turning up the volume” of your pain and therefore must be considered as well.
Even if you appear outwardly fit and strong, there’s a high probability that you have some degree of weakness in your spine.
Finally, degeneration of your discs and arthritis in your spine is not just the result of “wear and tear.” It may be because you haven’t had enough “wear and repair” in your lifetime. Sedentary people get just as much (and often much more) disc degeneration and osteoarthritis than active people do. (Osteoarthritis may, in fact, be a problem with a poor repair process rather than overuse.)
Remember that physical stress and loads placed on the body cause healthy adaptation. Load (activity), when appropriately applied, stimulates bone, disc, nerve, and muscle cells to produce healthy, strong tissues, and a strong back and neck.
For a downloadable copy of this blog, please click on the PDF link below.

Dr. David Olson
Contact Me